Understanding Prostate Cancer Treatment Guidelines
Prostate cancer is one of the most prevalent cancers affecting men worldwide. Early detection and effective treatment are crucial for managing the disease and improving patient outcomes. This article provides a comprehensive overview of prostate cancer treatment guidelines, offering detailed insights into the available options and factors influencing decision-making.
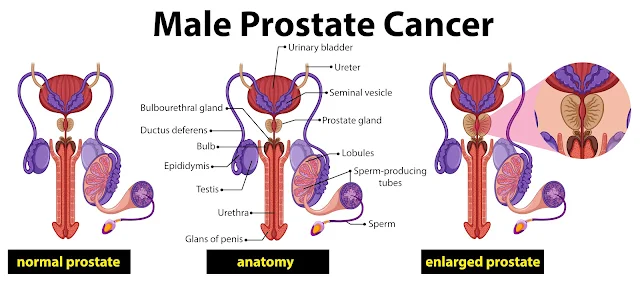
Overview of Prostate Cancer
Prostate cancer begins in the prostate gland, a small walnut-shaped organ that produces seminal fluid. While many cases progress slowly, others can be more aggressive and require prompt intervention. The cancer’s stage, grade, and specific characteristics play a critical role in determining the appropriate treatment path.
Early Detection and Diagnosis
Early detection is key in the management of prostate cancer. Screening typically involves a Prostate-Specific Antigen (PSA) test and a Digital Rectal Exam (DRE).
An elevated PSA level may indicate the presence of cancer, but further diagnostic tests, such as a biopsy or MRI, are required for confirmation.
Risk Stratification
Once prostate cancer is diagnosed, it is essential to stratify the risk to tailor treatment strategies.
The risk categories—low-risk, intermediate-risk, and high-risk—are determined based on PSA levels, Gleason score, and the extent of cancer spread.
- Low-risk prostate cancer is typically localized and grows slowly. Patients may not require immediate treatment and can be monitored through active surveillance.
- Intermediate-risk prostate cancer may necessitate more aggressive treatment, such as radiation therapy or surgery.
- High-risk prostate cancer requires immediate and comprehensive treatment, often involving a combination of therapies.
Treatment Options for Prostate Cancer
Active Surveillance
For patients with low-risk prostate cancer, active surveillance is often the preferred approach.
This strategy involves regular monitoring through PSA tests, DREs, and periodic biopsies.
Treatment is initiated only if the cancer shows signs of progression.
Active surveillance minimizes unnecessary treatment and preserves quality of life.
Surgery: Radical Prostatectomy
A radical prostatectomy involves the complete removal of the prostate gland and surrounding tissues.
It is a common option for patients with localized prostate cancer. The surgery can be performed through various techniques:
- Open Radical Prostatectomy: Traditional surgery with an incision in the lower abdomen.
- Laparoscopic Radical Prostatectomy: Minimally invasive surgery with smaller incisions.
- Robotic-Assisted Laparoscopic Prostatectomy: Utilizes robotic technology for enhanced precision.
Post-surgical outcomes depend on the cancer's stage and the patient’s overall health.
Nerve-sparing techniques may help preserve erectile function, though urinary incontinence is a potential side effect.
Radiation Therapy
Radiation therapy is a non-invasive option that uses high-energy rays to target and destroy cancer cells.
It is suitable for patients with localized prostate cancer or as an adjunct to other treatments in advanced cases. Two primary types of radiation therapy include:
- External Beam Radiation Therapy (EBRT): Delivers radiation from outside the body, targeting the prostate gland.
- Brachytherapy: Involves placing radioactive seeds directly into the prostate tissue, offering a high dose of radiation with minimal impact on surrounding organs.
Hormone Therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), reduces the levels of male hormones (androgens) that fuel prostate cancer growth.
It is often used in conjunction with radiation therapy or as a treatment for advanced prostate cancer.
Hormone therapy options include:
- Luteinizing Hormone-Releasing Hormone (LHRH) Agonists: Drugs that lower testosterone production.
- Anti-androgens: Medications that block the effects of testosterone on cancer cells.
- Orchiectomy: Surgical removal of the testicles to reduce androgen levels.
Hormone therapy can effectively slow cancer progression, but it is associated with side effects such as hot flashes, reduced libido, and bone thinning.
Chemotherapy
Chemotherapy is typically reserved for advanced prostate cancer that has spread beyond the prostate gland.
It involves the use of drugs that kill rapidly dividing cancer cells.
Chemotherapy is often combined with hormone therapy to enhance its effectiveness.
Common chemotherapy drugs include docetaxel and cabazitaxel.
Immunotherapy
Immunotherapy harnesses the body’s immune system to fight prostate cancer.
Sipuleucel-T is an FDA-approved immunotherapy for metastatic prostate cancer that has not responded to hormone therapy.
This treatment involves collecting immune cells from the patient, modifying them to target cancer, and re-infusing them into the body.
Immunotherapy is generally well-tolerated but may not be suitable for all patients.
Targeted Therapy
Targeted therapy involves drugs that specifically target cancer cells without affecting normal cells.
PARP inhibitors, such as olaparib and rucaparib, are examples of targeted therapies used for prostate cancer patients with specific genetic mutations (e.g., BRCA1/2).
These therapies are particularly effective in patients with advanced or metastatic cancer who have exhausted other treatment options.
Factors Influencing Treatment Decisions
Patient’s Age and Health Status
The patient’s age and overall health status are critical factors in treatment decisions.
Younger, healthier patients may benefit from aggressive treatments like surgery or radiation, while older patients with comorbidities may opt for less invasive options.
Cancer Stage and Grade
The stage and grade of prostate cancer heavily influence the treatment plan.
Early-stage cancers may be managed with active surveillance or localized treatments, whereas advanced-stage cancers require a multimodal approach.
Potential Side Effects
The potential side effects of each treatment option must be carefully weighed.
For instance, surgery carries risks of urinary incontinence and erectile dysfunction, while hormone therapy may lead to hot flashes and bone loss.
A personalized approach ensures that the chosen treatment aligns with the patient’s preferences and lifestyle.
Emerging Treatments and Clinical Trials
Advances in prostate cancer research are continually improving treatment outcomes.
Clinical trials offer access to cutting-edge therapies and novel drugs that are not yet widely available.
Patients should consult with their healthcare providers about the possibility of participating in clinical trials, especially if standard treatments are no longer effective.
The Importance of a Multidisciplinary Approach
Prostate cancer treatment often involves a multidisciplinary team of specialists, including urologists, oncologists, radiologists, and nurses.
This collaborative approach ensures that all aspects of the patient’s health and well-being are considered when devising a treatment plan.
Regular communication between the patient and healthcare team is vital for navigating the complexities of prostate cancer treatment.
Conclusion: Making Informed Decisions
Understanding prostate cancer treatment guidelines is essential for making informed decisions about care.
Each patient’s journey is unique, and treatment should be tailored to individual circumstances.
By staying informed about the latest advancements and consulting with a trusted healthcare team, patients can confidently navigate their treatment options and work towards the best possible outcomes.